Also known as … Capillary Malformation in modern terminology, as well as Nevus Flammeus
A port-wine stain is a pink to red flat patch on the skin which has well-defined edges. It is a true birthmark present in 3 to 5 per 1000 newborn babies. It is permanent and its area will increase in proportion to general body growth.
Port-wine stain should not be confused with other pink patches present at birth such as the stork bite mark. The stork bite mark (angel’s kiss, salmon patch) on the central forehead is very common and will usually go away by itself in the first or second year of life.
Port-wine stain is in the family of disorders known as vascular malformations. These are not the same as the far more common infantile haemangioma (strawberry birthmark) which is in the family of benign vascular tumours. Infantile haemangiomas are not usually present at birth. They have an early growth phase, become raised, and eventually shrink and disappear.
Our understanding of the condition remains limited. The birthmark is thought to be due to a disturbance in the behaviour of blood vessels. The nerve control of blood flow is deficient and this results in blood flow being at maximum all the time. The capillaries within the port-wine stain remain wide open and this produces the typical red appearance.
Normal skin will become red, for example, after sunburn, as a result of increased blood flow into the area. However, once the burn heals the blood vessels reduce to normal flow and the redness disappears. This normal behaviour cannot occur in a port-wine stain.
Recently an abnormality in the GNAQ gene has been discovered in port-wine stain areas. However, this will need further corroborative studies.
Port-wine stain is not hereditary.
At birth, the port-wine stain is typically pink to red. Although it is most commonly seen on the face, it can be present on any part of the body. In some cases the port-wine stain will thicken and become darker in colour later in adult life. The thickening can be in the form of small dark lumps or the whole stain may thicken.
Port-wine stain can be associated with certain syndromes. However, it is important to understand that the port-wine stain does not cause the syndrome but is simply a symptom of the condition.
- Klipell-Trenaunay syndrome (KTS): This condition combines a port-wine stain on an enlarged limb (usually a leg) with varicose like veins and swollen, irregular lymphatic vessels.
- Sturge-Weber syndrome: In this condition a port-wine stain is present on the face, usually involving the outer forehead, cheek and skin around the eye. Other features include epilepsy, glaucoma (an eye abnormality) and sometimes mental disability. In this syndrome abnormal blood vessels are present on the membranes that cover the brain.
The diagnosis is usually obvious from the appearance of the stain and a history of presence at birth without further disproportionate growth. Further investigations will be required if an associated syndrome is suspected.
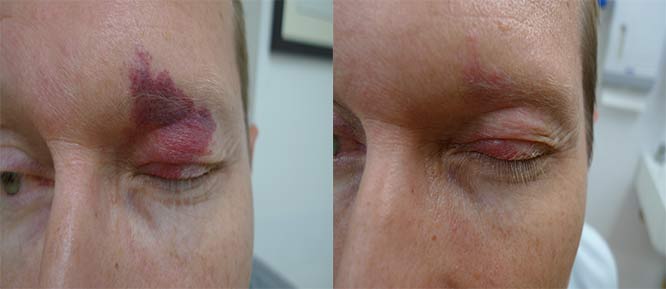
Port-wine stain can be treated with laser. The specific laser used depends on whether the stain is in the flat pink stage or the bluish thickened appearance that sometimes develops in older adults.
Treatment of flat pink childhood port-wine stain
Treatment is recommended, particularly if the port-wine stain involves the face as it can be associated with teasing at school. Treatment is best commenced as early possible as multiple treatment sessions are necessary. If a general anaesthetic is needed, this risk needs to be considered.
- Pulsed dye laser is the best established treatment for flat port-wine stain in infants and children. In 80% of cases, the stain lightens by at least 50%, with about 20% of port –wine stains becoming 80% lighter. Unfortunately, there is a group of between 10 and 20% of affected children who do not show a useful response to this treatment.
There is a trend to commence treatment as soon as possible after birth. Treatment is initially given at intervals of between 2 to 4 weeks. Under the age of about 4 months this can be done without general anesthetic as the treatment is not particularly painful. As children become older, treatment generally requires general anesthetic.
Treatment of adult-type thicker darker lesions
Thicker lesions may be more resistant to treatment. They require more deeply penetrating laser and light systems. Depending on availability and preference, these systems include long pulsed Alexandrite laser, long pulsed Nd: YAG laser and some IPL systems.
Safety of laser treatment
Treatment of childhood port-wine stains has a very high safety profile with the use of modern lasers that have skin cooling. There are very rare instances of minor blistering and scarring. The more deeply penetrating lasers, as used in adult stains, carry a slightly higher risk of minor scarring.
This information has been written by Dr Philip S Bekhor and Dr Davin S Lim
Disclaimer
2019 © Australasian College of Dermatologists.
You may use for personal use only. Please refer to our disclaimer.