What is mucous membrane pemphigoid?
Mucous membrane pemphigoid, previously known as cicatricial pemphigoid, is a very rare subepidermal autoimmune blistering disease which predominantly affects the mucous membranes such as the inner linings of the mouth, eyes and genitalia. The second part of its name, “pemphigoid”, comes from the Greek word pemphix, meaning bubbles. The incidence of mucous membrane pemphigoid is approximately 1.3 to 2.0 new cases per million people per year.
What causes it?
There are two main layers of the skin, the epidermis (the very top layer) and the dermis (the deep layer). The area between these layers is known as the basement membrane zone. Mucous membrane pemphigoid occurs when cells of the body’s immune system produce proteins (autoantibodies) that attack and damage the basement membrane zone. If these components are damaged, the two layers of the mucosal epithelium (body linings) break apart, causing blister formation. What causes the immune attack on the epithelium is unknown.
What does it look like?
The natural history of mucous membrane pemphigoid is not well understood as only a few small case series have been published. Females may be more commonly affected than males.
Mucous membrane pemphigoid most frequently affects the oral cavity (85% of affected individuals) followed by the eye (65% of affected individuals). Other sites of involvement include the skin, nose, rectum, pharynx, larynx, oesophagus, penis and vagina.
When mucous membrane pemphigoid is confined to the oral cavity, the disease tends to run a milder course with a higher chance of recovery when compared to other forms of mucous membrane pemphigoid. The oral lesions can manifest as patches, blisters or erosions. The condition often affects the gums (gingivae) (Figure 1) but may affect the palate and tongue and other mucosal surfaces.

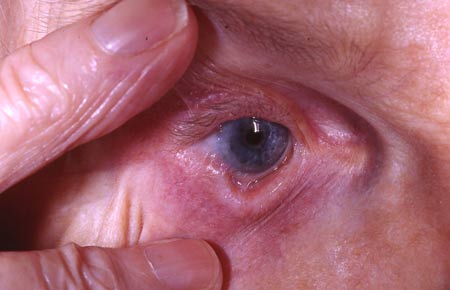
When mucous membrane pemphigoid is confined to the eye, the disease may be more aggressive, with a poor chance of recovery. It is sometimes termed “ocular pemphigoid” or “ocular cicatricial pemphigoid”. It usually starts with dryness, stinging or burning in one eye. It may be confused with other eye conditions, including ocular rosacea and dry eye syndrome, so it is important for these patients to have ongoing follow up with an ophthalmologist experienced in anterior ocular surface disease, ideally. Eventually, erosions start to form and the disease progresses to affect both eyes. It can result in various eye complications including tethering of the eyelid to the surface of the eye, known as symblepharon (Figure 2), ingrowing eyelashes which can irritate and scar the cornea, leading to blindness with debilitating effects on quality of life. As these complications cannot be reversed, early detection of ocular MMP is vital and early systemic treatment to halt progression and prevent scarring is vital.
Mucous membrane pemphigoid needs to be distinguished from other blistering conditions including pemphigus vulgaris, paraneoplastic pemphigus and Stevens-Johnson syndrome (SJS).
What other problems can occur with this condition?
Given the rarity of mucous membrane pemphigoid, there is insufficient evidence regarding its associations. A study has found that a particular subtype of mucous membrane pemphigoid (anti-laminin 332) may be associated with a solid cancer which was present in about 30% of affected individuals.
How is it diagnosed?
- Skin or mucosal biopsies – biopsy of the edge of a blister for routine pathology; biopsy of skin close to a blister can be sent for direct immunofluorescence which looks for deposition of the autoantibodies in the skin.
- Blood tests – these test for autoantibodies in the blood and are adjunctive to the biopsies, not a substitute for them.
How is it treated?
Treatment depends on the site of involvement. All affected individuals need to be seen by an ophthalmologist because of the risks of developing eye disease, whether or not they are symptomatic.A cancer screen may be needed in a small subgroup of patients.
Individuals with mild oral disease
Individuals with ocular or more aggressive disease
Systemic medications are often required. These can include:
- The best evidence from a Cochrane review was that mild disease performed best with oral dapsone, but that severe disease responded to cyclophosphamide. Often, prednisone is ineffective.
- Other Immune suppressants have been reported anecdotally, such as azathioprine, mycophenolate, cyclosporin, intravenous immunoglobulin and rituximab.
What is the likely outcome of this condition?
Mucous membrane pemphigoid tends to run a chronic course and long-term follow up is usually necessary. The disease activity may fluctuate at times.
The aim of treatment is to manage the disease to prevent long-term problems caused by scarring. Individuals with mucous membrane pemphigoid localised to the mouth generally have a better outcome with lower risks of scarring. However, individuals with eye involvement generally tend to have a more aggressive disease and a higher propensity to scar, resulting in eyelid adhesions and potential blindness. Eyelashes which start to grow inwards need to be removed either by plucking or lasering to destroy the follicles in order to prevent corneal damage.
This information has been written by Dr Cathy Zhao and Professor Dedee Murrell
Last updated: April 2023
Disclaimer
2019 © Australasian College of Dermatologists.
You may use for personal use only. Please refer to our disclaimer.